When Parents Need Support Too: Managing Your Own Anxiety
- Caroline Monteiro
- Jun 5
- 7 min read
Updated: Jul 15
Practical strategies for parents to manage their own stress while supporting their child.

At that point, I had been a nurse in a Paediatric ICU for over five years. I thought I had seen it all.
But some moments leave marks you don’t ever forget.
I was standing outside the isolation room. Inside was a little girl who had been two years in remission from leukemia, until she wasn’t. The relapse was sudden. Aggressive. She landed in ICU after complications from chemo.
I was outside the room when her grandmother came in to take over for the night.
Her mother stepped out quietly, not wanting to disturb her daughter’s rest. She closed the door behind her and turned.
And then she looked up with a pale and lost stare. She looked at me, her eyes wide, trying to stay composed, but I could see it. The raw fear behind her polite nod. The thousand worries bubbling just under the surface.
It was like someone unplugged her. Her body folded. She leaned against the wall like it was the only thing holding her up.
I walked in her direction and said gently, “It’s okay to take a breath. You can step away for a minute.”
She nodded once, and tears started rolling down her face. She hugged me like she hadn’t breathed in days.
And then she cried. Hard.
Not the quiet tears you dab away quickly. Not the kind you apologize for. These were full-body sobs. The kind that shake your spine. The kind you only let out when you feel helpless.
“I’m so scared,” she whispered. “I hate that she has to go through this again. I hate that I can’t fix it.”
I didn’t have answers. I just held her.
And in that moment, more than ever, I saw something that’s easy to forget in busy shift days and long treatment plans:
Parents need support, too.
Just because you’re the grown-up…Just because you’re the one packing the hospital bag and explaining blood tests and answering questions with a brave voice…Doesn’t mean you’re not terrified inside.
Your nervous system matters.Your exhaustion matters.Your trauma matters.
You are not just the support system. You are a human being who needs holding, too.
And that’s what this post is about.
Because your healing matters just as much as your child’s.
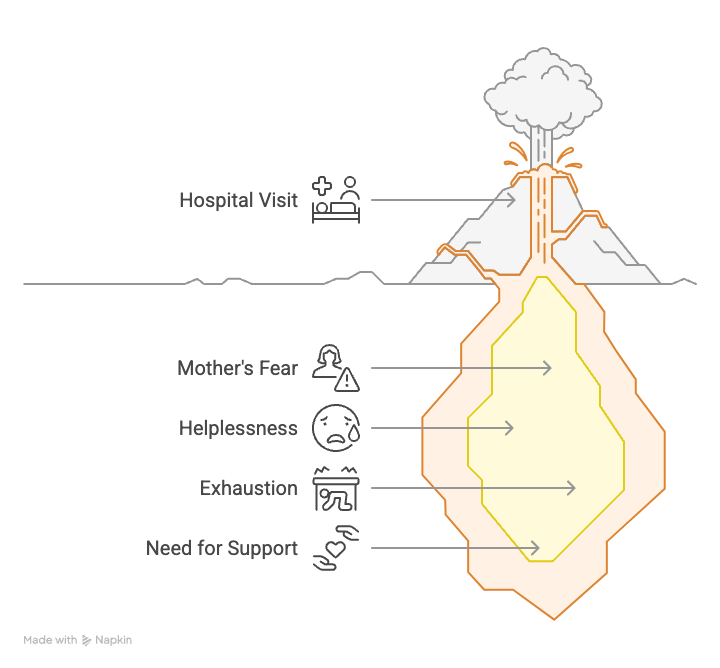
The Unseen Impact on Parents
When a child is facing a medical crisis or living with a chronic condition, the focus (understandably) is on their treatment, symptoms, and healing.
But the truth is, parents often walk parallel to that pain, carrying it in their body, absorbing it into their nervous system, and holding it all in so their child feels safe.
According to pediatric health experts and trauma researchers, it’s not uncommon for parents to experience symptoms of trauma and even post-traumatic stress disorder (PTSD) after witnessing or navigating repeated medical events with their child. In fact, research shows that up to 30% of parents of children admitted to Pediatric Intensive Care Units (PICUs) may meet the criteria for PTSD months after discharge. Some parents report:
Hypervigilance
Nightmares or insomnia
Avoidance of hospitals or reminders of the illness
Feelings of helplessness or guilt
Persistent anxiety, especially around health
It’s not a flaw. It’s a normal human response to an overwhelming situation.
You went into survival mode for your child. And sometimes, your nervous system doesn’t realize it’s allowed to come out of it.
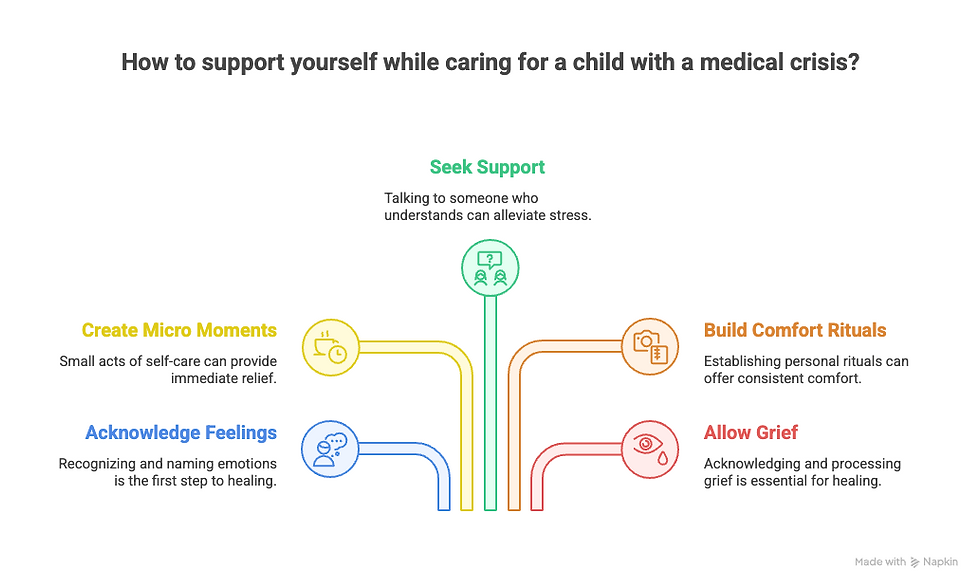
So What Can You Do?
Here are some practical, grounded ways to support yourself—because your well being shapes your child’s, too.
1. Name It Without Shame
Acknowledge what you're feeling. Saying "I'm anxious," "I'm overwhelmed," or even "I'm traumatized by what we went through" is not a weakness. It's a first step to healing.
According to pediatric health experts and trauma researchers, trauma isn’t just about what happened to you. It’s about what happened inside you as a result. Let yourself be honest about the impact.
Parents often dismiss their own emotions because they feel the focus should stay on their child. But here's the truth: healing starts with naming. You’re not being dramatic. You’re being human.
And when you say it out loud, or write it down, or whisper it into a pillow—you take back a little piece of power.
If your child had gone through what you have, would you tell them to 'just get on with it'? Of course not. You’d say, “Of course it hurts. Of course you’re tired. That makes sense.”
So say that to yourself.
Give yourself the same compassion you so freely give to your child.
2. Create Micro Moments of Safety
You might not be able to go on a holiday or take a full break. But you can:
Breathe deeply for 60 seconds
Sit in the car after an appointment with your eyes closed
Light a candle or sip a warm drink before bed
Put your phone away and watch the sky for five minutes
Place your hand on your chest and simply say, "I'm safe right now"
Wrap yourself in a soft blanket and let your shoulders drop.
Let’s imagine this:
You’ve just gotten through another morning of blood draws, vital checks, and hard conversations. The machines are quiet for once. Your child is asleep. You walk out into the corridor with a warm drink in hand. Not because it fixes anything, but because you need something gentle. You find a window. You stand still. You breathe. And for just one moment, it’s quiet inside you.
That’s the kind of pause we’re talking about.
It doesn’t need to be poetic. Or perfect. Or even every day.
Just real.
A breath. A sip. A single, kind moment when the world doesn’t need anything from you.
And that’s enough to start helping your body feel safe again.
“I don’t talk to anyone,” a mom once told me. “I just stand there and breathe. That’s my ten minutes.”
Those ten minutes mattered.
These tiny acts signal to your body: It’s safe to rest.
They’re not “just” little things. They are lifelines. When repeated, they teach your nervous system to soften again. To stop bracing. To slowly, gently trust that it doesn’t have to stay on high alert forever.
Because healing isn’t a grand gesture. It’s a series of quiet returns to safety.
3. Talk to Someone Who Gets It
Find someone who can listen without trying to fix you, whether that’s a counselor, another parent who understands, or even someone on the hospital staff who feels safe. Medical trauma isn’t just something that happens to children. It impacts everyone around them, especially the ones holding it all together.
Some parents tell me the best support they ever received came from a quiet cup of tea with another mum in the waiting room. Or the hospital social worker who remembered their name. Or a parent group where no one had to explain the weight they were carrying, because everyone just knew.
At Brave Nest, we understand that kind of quiet, non-judgmental support makes all the difference. That’s why we offer gentle, guided spaces for connection, whether that’s through our online community, one-to-one parent sessions, or self-paced emotional support tools built specifically for medical parents.
You don’t have to figure this out alone. Your story deserves space. Your emotions deserve attention. And your healing deserves time.
4. Build Your Own Comfort Rituals
We often build comfort kits for kids. But parents need touchpoints, too—small reminders that you are more than what you’re managing.
Try adding:
A journal, just for your thoughts, not the to-do list
A playlist that calms your nerves or uplifts you, depending on the day
A photo that reminds you of a time you felt strong or grounded
Your favorite hand cream or essential oil that brings comfort
A token from your child: a drawing, a small toy, even a note with their handwriting
These aren’t luxuries. They’re cues of care. Sensory anchors that bring you back to your own body when everything feels like too much.
Keep it somewhere you can reach for it easily—in your bag, in the glovebox, or in that drawer by the hospital bed.
And if you’re not sure what would soothe you, think about what you’d pack for someone you love.
Then do the same for yourself.
There’s no one-size-fits-all version. Some parents tuck in tea bags and prayer cards. Others pack fidget toys, lip balm, or scent sachets.
Whatever brings you even a few seconds of peace is worth including.
This is about making space to be a person, not just a parent under pressure.
5. Know That It’s Okay to Grieve
Even if your child is doing better now. Even if you made it through. Even if everyone around you says, “You’re so strong.”
You’re allowed to mourn what was lost: a sense of safety, a carefree childhood, the version of life you imagined before it all changed. You’re allowed to grieve birthdays that weren’t celebrated, milestones that were delayed, and holidays spent in waiting rooms instead of at home.
Sometimes that grief hides under frustration or numbness. Sometimes it bubbles up in quiet moments when no one else is watching.
One mum once told me she didn’t cry during the whole hospital stay and treatment. She was “too busy holding it all together.” But three months after discharge, she broke down in a supermarket aisle. Over a box of cereal. “I realized we were out of the one she ate after every chemo session,” she said. “And it just… shattered me.”
That’s what grief looks like sometimes. It’s sneaky. Tender. Unexpected.
Healing doesn’t mean ignoring the pain. It means giving it room to breathe. It means saying, “This was hard,” and letting that be true without needing to fix it.
It means acknowledging that the road changed you, and allowing space for that story to live in your body without shame.
Grief isn’t a detour. It’s part of the path forward.
You Deserve Support, Too
You are not just a caregiver. You are a parent. A person. And you matter.
Let this be your reminder that your healing is part of your child’s care plan.
There is no gold medal for suffering in silence.
Take the breath. Cry the tears. Ask for help.
And know, deep in your bones, that you don’t have to do this alone.
Because brave kids are raised by brave parents. And bravery includes taking care of yourself, too.
If this resonated with you, we invite you to download our free resource: “Moments of Calm: 10 Simple Practices for Parents in Medical Crisis.” It’s a gentle guide to help you find steadiness, even in the storm. You can find it in our Brave Nest resource library.



Comments